People Profile – Dr. Adam Hood
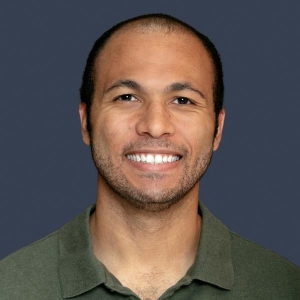
Adam Hood, MD, (PGY 2; Family Medicine)
Adam Hood, MD, (PGY 2; Family Medicine) says the beauty of family medicine is being able to make a significant impact in a patient’s life by taking an interest in who they are and attempting to understand and treat the person, not just the disease.
As a family medicine resident at MedStar Health–Georgetown/Washington Hospital Center, Dr. Hood describes his day-to-day as taking care of patients, in both inpatient and outpatient settings, across all walks of life and all demographics—everyone from pregnant patients and their babies to young children and the elderly. Being able to interact with and serve so many different types of people is what Dr. Hood loves most about his job.
This aspect of his work, however, has also helped shape his hope for the future of medicine in the United States—one where there is greater health equity. Dr. Hood acknowledges that a lot of good work has already been done on this front, but there is still significant progress to be made.
“I have patients who have to choose between paying for medications or paying for food or rent, or who would benefit from a certain medication but, because of their insurance or lack of insurance, aren’t able to afford it,” he says.
While Dr. Hood may have briefly considered careers outside of medicine—or even other specialties—where he landed may have, ultimately, been predestined. After all, both of his parents are primary care physicians in his hometown of Lubbock, Texas.
Prior to beginning his residency at MedStar Health, Dr. Hood says he had never lived outside of the state of Texas. But he emphasizes how fortunate he feels to have ended up in his program, where, he says, everyone is committed to helping each other become the best family medicine physicians they can be. He’s also thankful for his cohort of supportive residents, who help each other grow personally and professionally.
Dr. Hood says that his cohort regularly checks in with each other, whether through quick texts or more intense heart-to-hearts, and the advice he offers his fellow residents is to make sure they are prioritizing their health.
“Our jobs are to focus on the health of others, so our own health and well-being can get brushed to the side. You will be the best version of yourself as a doctor if you prioritize your own physical and mental health. As one of our attendings, Dr. Kirk, likes to say, ‘You can’t pour from an empty cup.’”
Outside of work, Dr. Hood “fills his cup” by staying active, exploring all of DC’s amazing parks and museums with his wife, and discovering new area restaurants.















