People Profile – Dr. Claudia Georges

Claudia Georges’, MD, (Junior Academic Faculty/Chief Resident)
Claudia Georges’, MD, (Junior Academic Faculty/Chief Resident) curiosity for science and interest in helping others are the driving forces behind her passion for medicine. As a student, she was fascinated by the human body and how it functions; her interest in science deepened with every biology class and science fair. This interest soon became a passion when she realized she could use her medical skills to help the most vulnerable.
Born in Syria, Claudia moved to the DMV (DC/Maryland/Virginia area) to complete her residency. During her time in medical school, the war in Syria displaced families, leaving them without access to healthcare. This was devastating for Claudia – she knew she had to act. Claudia volunteered to help by offering psychological support to displaced families and their children. This was a profound experience for her, reinforcing her belief that “medicine is much more than treating illness.”
Claudia’s reach and impact on the health of communities is not restricted by arbitrary, geological lines drawn on a map. She leverages her expertise and skillset to benefit local communities in the DMV, and to push for innovation and healthcare change across the entire United States. She envisions a future where medicine in the United States is more personalized and patient centered, noting that to provide the best care possible, physicians must take the time to understand and listen to their patients. Claudia explains that “Every patient has a story!”
Claudia is optimistic about the future of healthcare in the United States. She looks forward to a healthcare model that puts a greater emphasis on preventive care, addressing health disparities, and social determinants of health. Positive change takes leadership – luckily, we have Claudia.
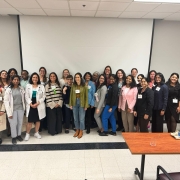
Since beginning her residency at MedStar Health Baltimore, she has envisioned creating an alumni association. This association helps foster a strong sense of community, offers professionals a network of support, mentorships, research opportunities, and drives collaboration – giving physicians and residents the skills and resources they need to provide quality care to the communities they serve. As a credit to her persistence and hard work, more than 130 alumni have joined the newly launched MHIM Baltimore Alumni Association. (Click here to join!)
Collaboration in medicine leads to better health outcomes. Leaders like Claudia help to effectuate this change. Claudia practices what she preaches: “Instead of merely observing, we must step up as leaders to drive change, as our world needs more leaders now than ever.”