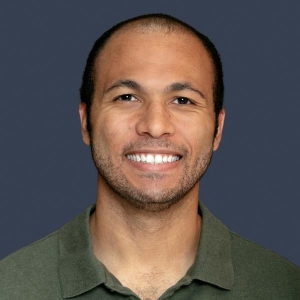
People Profile – Dr. Flavia Tejada Frisancho

Flavia Tejada Frisancho, MD, (PGY 2; Internal Medicine)
For Flavia Tejada Frisancho, MD, (PGY 2; Internal Medicine), leaving her home country of Peru to pursue her dreams may not have been easy. But every challenge has made her stronger, she says, and she hopes to inspire others—especially women and minorities in medicine—to chase their goals fearlessly.
Medicine has always been a part of Dr. Tejada Frisancho’s life and her family’s story. Her grandfather, a surgeon, met her grandmother, a scrub nurse, right in the operating room. And Dr. Tejada Frisancho was born during her parents own medical residencies—her mom’s in ophthalmology and her dad’s in oncology/head and neck surgery. (“Honestly, I have no idea how they managed—shoutout to all the parents going through residency!” she adds.)
Seeing firsthand the impact her parents had on their patients, Dr. Tejada Frisancho knew she wanted to dedicate her life to something just as meaningful. She says the cherry on top was getting to apply science—her favorite subject—to real life in the most impactful way.
“I always thought I would follow in my family’s footsteps and pursue a surgical specialty. After all, surgery is practically in my DNA,” she says. “But during medical school, everything changed when I rotated through internal medicine, especially critical care and cardiology.”
Dr. Tejada Frisancho loved the critical thinking required in internal medicine and, sometimes, the opportunity to play detective. She also liked the chance to build long-term relationships with her patients and advocate for them throughout their journey.
Dr. Tejada Frisancho says the unwavering support from her program, mentors, and colleagues has helped her succeed at MedStar Washington Hospital Center. She appreciates that MedStar Health encourages growth and innovation, whether through hands-on learning, participating in committees, or engaging with diverse patient populations, and she’s eager to pursue opportunities to be more involved this year.
“I believe that leadership and advocacy are essential in medicine, and I Iook forward to finding ways to contribute beyond clinical care,” she says.
Along with her residency program’s book club, Dr. Tejada Frisancho is currently reading “The Picture of Dorian Gray” by Oscar Wilde. “It explores vanity and the consequences of unchecked ambition—something that can even resonate in medicine at times!” she says. When she’s away from the hospital, Dr. Tejada Frisancho also enjoys painting and loves to explore art galleries and discover local artists.








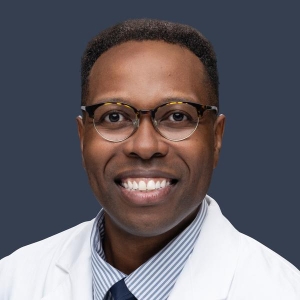 A heartfelt congratulations to Dr. Muwanga (PGY-1, D.C. General Surgery Program) for his unwavering dedication to our patients! A grateful family nominated him for a SPIRIT Award, recognizing his exceptional care and describing him as “kind, cheerful, professional, and incredibly polite.”
A heartfelt congratulations to Dr. Muwanga (PGY-1, D.C. General Surgery Program) for his unwavering dedication to our patients! A grateful family nominated him for a SPIRIT Award, recognizing his exceptional care and describing him as “kind, cheerful, professional, and incredibly polite.”